Glycoconjugates, complex molecules composed of carbohydrates linked to proteins or lipids, have emerged as powerful tools in modern medicine. These versatile compounds play crucial roles in cellular recognition, signaling, and immune responses, making them invaluable targets for therapeutic interventions.
Structural diversity of therapeutic glycoconjugates
The remarkable diversity of glycoconjugate structures provides a vast array of possibilities for therapeutic applications. These molecules can be broadly categorized into glycoproteins, glycolipids, and glycosaminoglycans, each with unique structural features that contribute to their specific functions in the body and their potential as therapeutic agents.
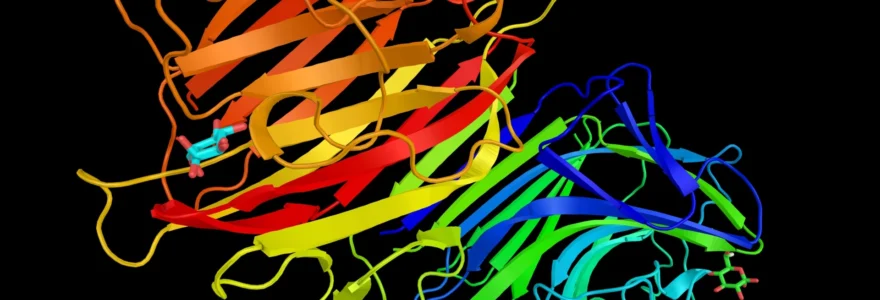
Glycoproteins, characterized by carbohydrate chains attached to protein backbones, exhibit a wide range of glycosylation patterns . The nature, number, and position of these sugar moieties can significantly influence the protein's stability, half-life, and biological activity. This structural variability allows for fine-tuning of glycoprotein-based drugs to optimize their therapeutic properties.
Glycolipids, consisting of carbohydrate chains linked to lipid molecules, play crucial roles in cell membrane organization and signaling. Their unique structures make them particularly valuable in developing treatments for lysosomal storage disorders and as components of targeted drug delivery systems.
Glycosaminoglycans, long unbranched polysaccharides often found attached to proteins to form proteoglycans, are essential components of the extracellular matrix. Their diverse structures, ranging from heparin to hyaluronic acid, provide a rich source of therapeutic agents, particularly in the areas of anticoagulation and tissue regeneration.
The structural complexity of glycoconjugates is both a challenge and an opportunity in drug development, offering unprecedented specificity in targeting and modulating biological processes.
Glycoprotein-based therapeutics: from erythropoietin to monoclonal antibodies
Glycoprotein-based therapeutics have revolutionized the treatment of various diseases, leveraging the power of glycosylation to enhance drug efficacy and stability. These biologics range from hormones to complex monoclonal antibodies, each utilizing specific glycosylation patterns to optimize their therapeutic effects.
Recombinant erythropoietin (EPO) in anemia treatment
Erythropoietin, a glycoprotein hormone crucial for red blood cell production, exemplifies the importance of glycosylation in therapeutic proteins. Recombinant EPO, used to treat anemia associated with chronic kidney disease and chemotherapy, relies heavily on its glycosylation profile for optimal pharmacokinetics and biological activity.
The sialic acid content of EPO's glycan structures directly correlates with its serum half-life and in vivo activity. By engineering EPO with additional glycosylation sites, researchers have developed hyperglycosylated variants with extended half-lives, allowing for less frequent dosing and improved patient outcomes.
Glycoengineered monoclonal antibodies for enhanced effector functions
Monoclonal antibodies represent a rapidly growing class of glycoprotein therapeutics, with applications ranging from cancer treatment to autoimmune disease management. The glycosylation pattern of antibodies, particularly in the Fc region, profoundly influences their effector functions, including antibody-dependent cell-mediated cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC).
Glycoengineering techniques have enabled the development of antibodies with optimized glycosylation profiles. For instance, afucosylated antibodies exhibit enhanced ADCC activity, making them more potent in targeting cancer cells. This approach has been successfully applied in the development of several approved therapeutic antibodies, significantly improving their clinical efficacy.
A notable example is the development of glycoengineered antibodies for cancer therapy. These modified antibodies have shown increased binding affinity to Fc receptors on immune cells, resulting in more robust anti-tumor responses. You can find more detailed information on glycoconjugate structures and their therapeutic applications at elicityl-oligotech.com , which provides comprehensive resources on this topic.
Follicle-stimulating hormone (FSH) glycoforms in fertility treatments
Follicle-stimulating hormone, another crucial glycoprotein hormone, plays a vital role in fertility treatments. The glycosylation pattern of FSH significantly affects its receptor binding and signal transduction properties. By manipulating the glycosylation profile of recombinant FSH, researchers have developed variants with improved pharmacokinetics and biological activity.
These glycoengineered FSH preparations have shown enhanced efficacy in stimulating follicular development and oocyte maturation, leading to improved outcomes in assisted reproductive technologies. The ability to fine-tune the glycosylation of FSH exemplifies how glycoengineering can be leveraged to optimize hormone therapies.
N-linked glycosylation patterns in therapeutic glycoproteins
N-linked glycosylation, where sugar chains are attached to asparagine residues in proteins, is a critical feature of many therapeutic glycoproteins. The complexity and composition of these N-glycans can significantly impact the protein's stability, immunogenicity, and biological activity.
Researchers have developed strategies to control and optimize N-glycosylation patterns in recombinant proteins. These include:
- Glycosylation site engineering to introduce or remove N-glycosylation sites
- Cell line selection and culture condition optimization to modulate glycan structures
- In vitro enzymatic remodeling of glycan chains post-production
- Use of glycosylation inhibitors to produce proteins with simplified glycan profiles
By carefully manipulating N-glycosylation, developers can create glycoprotein therapeutics with enhanced stability, reduced immunogenicity, and optimized pharmacokinetic properties, ultimately leading to more effective and safer medications for patients.
Glycolipid therapeutics: targeting lysosomal storage disorders
Glycolipid-based therapeutics have shown particular promise in the treatment of lysosomal storage disorders, a group of rare genetic conditions characterized by the accumulation of specific glycolipids in cellular lysosomes. These disorders result from deficiencies in enzymes responsible for glycolipid metabolism, leading to progressive cellular dysfunction and organ damage.
Glucocerebrosidase replacement therapy for gaucher disease
Gaucher disease, one of the most common lysosomal storage disorders, is caused by a deficiency in the enzyme glucocerebrosidase. This deficiency leads to the accumulation of glucocerebroside in lysosomes, particularly in macrophages, resulting in various clinical manifestations including hepatosplenomegaly, bone abnormalities, and hematological complications.
Enzyme replacement therapy using recombinant glucocerebrosidase has revolutionized the treatment of Gaucher disease. The therapeutic enzyme is modified with specific glycan structures to target it to macrophages, the primary affected cells in this disorder. This targeted delivery approach, utilizing the mannose receptor on macrophages, enhances the efficacy of the treatment while minimizing potential side effects.
Glycoengineering of therapeutic enzymes for lysosomal storage disorders has significantly improved their cellular uptake and lysosomal targeting, leading to more effective treatments for these devastating conditions.
Fabry disease treatment with recombinant α-galactosidase A
Fabry disease, another lysosomal storage disorder, is characterized by a deficiency in α-galactosidase A, leading to the accumulation of globotriaosylceramide in various tissues. The development of recombinant α-galactosidase A as an enzyme replacement therapy has markedly improved the management of this condition.
Similar to the approach used in Gaucher disease treatment, the recombinant enzyme for Fabry disease is glycoengineered to enhance its uptake by affected cells. The glycosylation pattern of the enzyme is optimized to facilitate its internalization via mannose-6-phosphate receptors, ensuring efficient delivery to lysosomes where it can catabolize the accumulated substrate.
Sphingolipid-based therapies for neurological disorders
Beyond enzyme replacement therapies, glycolipids themselves are being explored as potential therapeutic agents, particularly in the context of neurological disorders. Sphingolipids, a class of glycolipids abundant in neural tissues, play crucial roles in cell signaling and membrane organization.
Research into sphingolipid-based therapies has focused on several areas:
- Development of sphingolipid analogs as neuroprotective agents
- Use of glycosphingolipids as modulators of neuroinflammation
- Exploration of sphingolipid metabolism pathways as therapeutic targets in neurodegenerative diseases
- Application of sphingolipid-based nanoparticles for drug delivery across the blood-brain barrier
These approaches leverage the natural roles of sphingolipids in neural function to develop novel treatments for conditions such as Alzheimer's disease, Parkinson's disease, and multiple sclerosis. The unique properties of glycolipids in cellular membranes and signaling pathways offer promising avenues for therapeutic intervention in complex neurological disorders.
Glycosaminoglycan-derived medications in thrombosis management
Glycosaminoglycans (GAGs), particularly heparin and its derivatives, have long been cornerstone therapies in the management of thrombosis and anticoagulation. The structural diversity of GAGs allows for the development of a range of anticoagulant medications with varying pharmacokinetic and pharmacodynamic profiles.
Low molecular weight heparins: enoxaparin and dalteparin
Low molecular weight heparins (LMWHs) represent a significant advancement in anticoagulation therapy. Derived from unfractionated heparin through controlled depolymerization, LMWHs offer several advantages over their parent compound, including more predictable pharmacokinetics, improved bioavailability, and a reduced risk of heparin-induced thrombocytopenia.
Enoxaparin and dalteparin, two widely used LMWHs, exemplify how modifications to the basic heparin structure can yield therapeutics with optimized properties:
- Enhanced subcutaneous bioavailability, allowing for outpatient administration
- Longer half-life, permitting once or twice daily dosing
- More predictable anticoagulant response, reducing the need for routine monitoring
- Reduced binding to plasma proteins and endothelial cells, leading to a more stable anticoagulant effect
These properties have made LMWHs the preferred anticoagulants for many clinical scenarios, including the prevention and treatment of venous thromboembolism in both medical and surgical patients.
Fondaparinux: A synthetic pentasaccharide anticoagulant
Fondaparinux represents a further refinement in GAG-based anticoagulant therapy. This synthetic pentasaccharide is designed to mimic the specific antithrombin-binding sequence of heparin, resulting in a highly selective inhibitor of Factor Xa. The development of fondaparinux illustrates how understanding the structure-function relationships of natural GAGs can lead to the creation of targeted synthetic analogs with improved therapeutic profiles.
Key advantages of fondaparinux include:
- Highly specific anticoagulant action, reducing off-target effects
- No risk of heparin-induced thrombocytopenia due to its synthetic nature
- Predictable linear pharmacokinetics, simplifying dosing regimens
- Long half-life allowing for once-daily subcutaneous administration
The success of fondaparinux has paved the way for the development of other synthetic GAG-based anticoagulants, demonstrating the potential of rational drug design in this field.
Heparin mimetics in development for anticoagulation therapy
Building on the success of LMWHs and fondaparinux, researchers are developing novel heparin mimetics with enhanced properties. These compounds aim to overcome some of the limitations of current GAG-based anticoagulants while retaining their beneficial effects.
Areas of focus in heparin mimetic development include:
- Creation of orally bioavailable heparin-like molecules
- Development of reversible, direct-acting anticoagulants based on GAG structures
- Engineering of multifunctional GAG mimetics with anticoagulant and anti-inflammatory properties
- Exploration of non-anticoagulant functions of heparin for therapeutic applications
These ongoing research efforts highlight the continued importance of GAG-based therapeutics in thrombosis management and their potential applications in other areas of medicine.
Glycoconjugate vaccines: enhancing immunogenicity against pathogens
Glycoconjugate vaccines represent a major advancement in vaccine technology, particularly for preventing infections caused by encapsulated bacteria. By coupling bacterial polysaccharides to carrier proteins, these vaccines elicit a T-cell dependent immune response, resulting in improved immunogenicity and long-lasting protection, especially in infants and young children.
Haemophilus influenzae type b (hib) conjugate vaccine
The Hib conjugate vaccine was a groundbreaking development in the prevention of invasive Haemophilus influenzae type b disease. By conjugating the capsular polysaccharide of Hib to a carrier protein, such as tetanus toxoid or CRM197 (a non-toxic mutant of diphtheria toxin), the vaccine induces a robust and long-lasting immune response even in young infants.
The success of the Hib conjugate vaccine has led to a dramatic reduction in Hib disease incidence worldwide, demonstrating the power of glycoconjugate technology in vaccine development.
Pneumococcal conjugate vaccines: PCV13 and PCV15
Building on the success of the Hib vaccine, pneumococcal conjugate vaccines have been developed to protect against Streptococcus pneumoniae infections. These vaccines conjugate multiple pneumococcal serotype-specific capsular polysaccharides to a carrier protein, providing broad protection against the most common disease-causing serotypes.
The evolution of pneumococcal conjugate vaccines illustrates the ongoing refinement of glycoconjugate technology:
- PCV7: First-generation vaccine covering 7 serotypes
- PCV13: Expanded coverage to 13 serotypes, including emerging pathogens
- PCV15: Latest formulation with protection against 15 serotypes
These vaccines have significantly reduced the incidence of invasive pneumococcal disease, particularly in children, and have demonstrated indirect protection in unvaccinated populations through herd immunity effects.
Meningococcal conjugate vaccines: Quadrivalent formulations
Meningococcal conjugate vaccines represent another significant application of glycoconjugate technology in preventing bacterial meningitis and septicemia. Quadrivalent formulations have been developed to provide protection against four major serogroups of Neisseria meningitidis (A, C, W, and Y).
These vaccines typically conjugate the capsular polysaccharides of each serogroup to a carrier protein such as diphtheria toxoid or CRM197. The quadrivalent approach offers several advantages:
- Broad coverage against multiple disease-causing serogroups
- Improved immunogenicity compared to plain polysaccharide vaccines
- Induction of immunological memory for long-lasting protection
- Potential for reducing nasopharyngeal carriage, contributing to herd immunity
The success of meningococcal conjugate vaccines has led to their inclusion in routine immunization programs in many countries, significantly reducing the incidence of invasive meningococcal disease.
Glycoconjugate malaria vaccines in clinical trials
The application of glycoconjugate technology in malaria vaccine development represents an exciting frontier in combating this global health threat. Researchers are exploring the use of malaria-specific glycan antigens conjugated to carrier proteins to elicit robust immune responses against the parasite.
Several glycoconjugate malaria vaccine candidates are currently in various stages of clinical trials. These vaccines target different stages of the Plasmodium life cycle, with a focus on preventing parasite invasion of red blood cells. Key approaches include:
- Conjugation of synthetic glycan epitopes mimicking P. falciparum surface antigens
- Use of native parasite glycans isolated and purified from cultured parasites
- Development of multivalent formulations targeting multiple parasite life stages
While challenges remain in achieving sufficient efficacy and durability of protection, glycoconjugate malaria vaccines hold promise for enhancing the global malaria control and elimination efforts.
Emerging glycoconjugate therapies in cancer treatment
The field of glycoconjugate therapies in oncology is rapidly evolving, offering new strategies for targeted drug delivery and immunotherapy. By leveraging the unique properties of glycans in cancer biology, researchers are developing innovative approaches to improve treatment efficacy and reduce side effects.
Antibody-drug conjugates: ado-trastuzumab emtansine and brentuximab vedotin
Antibody-drug conjugates (ADCs) represent a powerful class of targeted cancer therapies that combine the specificity of monoclonal antibodies with the cytotoxic potency of small molecule drugs. The glycosylation of the antibody component plays a crucial role in the pharmacokinetics and efficacy of these conjugates.
Two notable examples of successful ADCs are:
- Ado-trastuzumab emtansine (T-DM1): Targets HER2-positive breast cancer
- Brentuximab vedotin: Used in the treatment of CD30-positive lymphomas
In both cases, the glycosylation profile of the antibody influences its stability, half-life, and ability to interact with Fc receptors on immune cells. Optimizing the glycan structures on these ADCs can enhance their therapeutic index by improving drug delivery to tumor cells while minimizing off-target effects.
Glycosylated nanoparticles for targeted drug delivery
Glycosylated nanoparticles represent an innovative approach to targeted drug delivery in cancer treatment. By decorating nanoparticles with specific glycan structures, researchers can exploit the altered glycan-binding properties of cancer cells to achieve selective drug delivery.
Key advantages of glycosylated nanoparticles include:
- Enhanced tumor targeting through recognition of cancer-specific lectins
- Improved drug solubility and stability
- Potential for overcoming multidrug resistance mechanisms
- Reduced systemic toxicity compared to conventional chemotherapy
Ongoing research is exploring various glycan-nanoparticle combinations to optimize targeting efficiency and drug release kinetics for different types of cancer.
Tumor-associated carbohydrate antigens as immunotherapy targets
Tumor-associated carbohydrate antigens (TACAs) are aberrant glycan structures frequently expressed on cancer cells. These unique glycan signatures are being explored as targets for cancer immunotherapy, with several approaches under investigation:
- Development of anti-TACA monoclonal antibodies
- Creation of TACA-based cancer vaccines
- Design of chimeric antigen receptors (CARs) targeting TACAs
- Use of TACA-specific aptamers for targeted drug delivery
By targeting these cancer-specific glycan structures, researchers aim to develop more selective and effective immunotherapies with reduced off-target effects on healthy tissues.
Glycomimetic drugs interfering with selectin-mediated metastasis
Selectins, a family of carbohydrate-binding proteins, play a crucial role in cancer metastasis by facilitating the adhesion of circulating tumor cells to blood vessel walls. Glycomimetic drugs designed to interfere with selectin-mediated interactions represent a promising approach to prevent or reduce metastatic spread.
These glycomimetics typically mimic the natural ligands of selectins, competing for binding sites and disrupting the metastatic cascade. Potential applications include:
- Adjuvant therapy to reduce the risk of metastasis after primary tumor removal
- Combination therapy with conventional chemotherapeutics to enhance overall efficacy
- Prophylactic treatment in high-risk patients to prevent metastatic disease
Clinical trials of selectin-targeting glycomimetics are ongoing, with early results showing promise in reducing metastatic burden in various cancer types. As our understanding of the role of glycans in cancer biology continues to grow, so too does the potential for glycoconjugate-based therapies to revolutionize cancer treatment strategies.